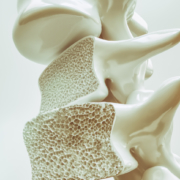
What’s the Difference Between Osteopenia and Osteoporosis?
Osteopenia and osteoporosis are two very similar conditions, but one is more severe than the other. Both conditions are decreased bone density, but osteopenia is to a lesser degree than osteoporosis. Osteopenia is still a problem though because it can increase a person’s chances of breaking a bone due to bone fragility.
What are the symptoms?
Osteopenia usually doesn’t cause symptoms unless a bone is broken. However, some patients who present with osteopenia complain of dull back pain.
Symptoms associated with osteoporosis include the following:
- Back pain, caused by a fractured or collapsed vertebra
- Loss of height over time
- A stooped posture
- A bone fracture that occurs much more easily than expected
What are the causes and who is at risk?
Women (primarily small-boned Caucasian and Asian) are most at risk for both conditions, primarily those who are age 65 or older as well as women who are postmenopausal. However, men can also be affected.
Anyone who meets any of the criteria for being at risk for either of the bone conditions should be evaluated. Often, catching the conditions early can make a significant difference in the effects that they have on the body and in some cases, can even be arrested so that they don’t progress.
Some of the common causes of both conditions include:
- Lifestyle habits
- Smoking
- Insufficient calcium
- Sedentary lifestyle
- Excessive alcohol consumption
- Vitamin D deficiency
- Carbonated beverages
- Medical situations
- Bulimia, anorexia, and other eating disorders
- Estrogen deficiency in women
- Certain hormone imbalances
- Overactive thyroid
- Certain treatments including radiation and chemotherapy
- Low testosterone in men
- Medications including anti-seizure, hydrocortisone, and steroids
- Health issues
- Tumors
- Cystic fibrosis
- Crohn’s disease
- Digestive issues
It should also be noted that certain types of diets, particularly those that advocate extremely low fat, or no fat can also cause problems. Vitamin D is necessary for calcium absorption in the body, but vitamin D is a fat-soluble vitamin meaning the body requires some fat in order to make use of it. When there is inadequate fat, the vitamin cannot be absorbed and in turn calcium cannot be absorbed.
A family history of osteopenia, osteoporosis, or low bone mass can increase a person risk by 50% to 85%.
How is it diagnosed?
Bone mineral density (BMD) tests are used to diagnose both osteopenia and osteoporosis by measuring the calcium levels in bone. This type of test can also provide an estimate of how much at risk a person is for bone fractures.
This test is painless and non-invasive. It is usually performed on the heel, shin bone, wrist, spine, finger, or hip.
Two common types of these tests are radiographs, a common diagnostic tool for osteopenia, and Dual Energy X-ray Absorptiometry (DEXA). A DEXA scan is essentially a low energy x-ray so patients are not exposed to as much radiation as they would be if they had a regular x-ray. The results are attained by comparing the score (measurements taken) to scans of individuals who do not have the condition.
Once the score is measured and compared, it is assessed using a chart that identifies the level or risk:
- +1.0 to -1.0 – Normal bone density
- -1.0 to -2.5 – Low bone density
- -2.5 or higher – At risk for osteoporosis
What are the treatments?
As with most conditions, prevention is the most effective treatment. If you have a family history or fall under any of the risk factors, there are things you can do to minimize the effects or prevent the conditions completely.
Your chiropractor can talk to you about lifestyle changes, exercise, and diet as well as supplements that you can take. Chiropractic adjustments can also be effective for many patients with osteopenia and osteoporosis as long as the choose technique is a low force technique like Activator.
Many patients find these natural treatments preferable to any medications that may be prescribed. The most important thing you should do, though, is get a bone density test if you are in an at-risk category, are a woman who is postmenopausal or age 65 or older.
To learn more about our office, check out our website @ ocwc.ca
[/av_textblock]